Can Doctors Prevent Overtreatment for Prostate Cancer Patients?
-
In a recent article in the Journal of the American Medical Association, entitled, “Overdiagnosis and Overtreatment in Cancer An Opportunity for Improvement,” a group of experts discussed the findings from a National Cancer Institute working group designed to improve the current approach to cancer screening and prevention1.
Among their recommendations included a motion to reclassify indolent or low-risk cancers as IDLE (indolent lesions of epithelial origin), so that patients are less likely to seek intensive treatments that may be potentially harmful.
While this narrative was designed to be provocative, it highlights the increasingly common debate regarding the over diagnosis and over treatment of screen detected or incidentally diagnosed cancers. While pervasive throughout oncologic care, over diagnosis and treatment of early stage, or “low risk,” prostate cancer has been publicly scrutinized and has received significant media attention.
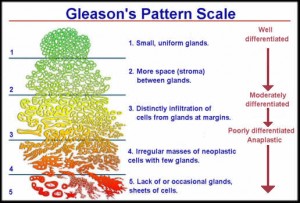
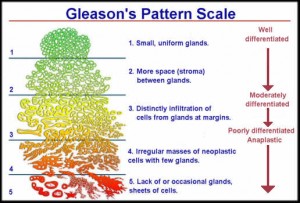
“Low risk” prostate cancer can be practically defined as low grade (Gleason Score ≤6), low volume (≤3 biopsy cores), non-palpable (negative digital rectal exam) disease with a PSA <10 ng/mL. These are thought to represent cancers with low malignant potential that are unlikely to impact a patient’s longevity. While the preferred management strategy historically has been immediate treatment with prostatectomy or radiation, the evidence is accumulating that at the population level, deleterious effects on quality of life (incontinence, impotence) may outweigh a marginal survival benefit if all patients with low risk disease undergo definitive therapy.
Acknowledging the concerning health policy implications of over diagnosis and treatment, prostate cancer remains the second leading cause of cancer death in men (behind lung cancer). Reclassifying men with Gleason 6 disease as “IDLE” is one approach to reduce the number of patients who carry a prostate cancer diagnosis, but this places a large number of men at risk, particularly if their initial biopsy under-sampled (or “missed”) a focus of more aggressive disease. Further, there are some patients with Gleason 6 cancers who will clinically progress, metastasize, and die of their disease. Currently, at the time of diagnosis we lack reliable tools to discriminate between early stage cancers that will remain indolent and those whose phenotype will aggressively transform over time.
In contrast, a more effective way of reducing over treatment is improving patient-provider communication regarding the risks and benefits of immediate treatment. Informed discussions accounting for patient preferences, tumor characteristics, competing risks, and life expectancy provides the opportunity to tailor treatment strategies for each individual patient. Put more simply, just because you were diagnosed with low risk prostate cancer does not mean that you need to undergo immediate treatment, there are alternative options.
Active surveillance with curative intent is a strategy that defers initial treatment in favor of close monitoring and reassessment of disease. Designed to defer (or avoid entirely) the side effects incurred with local therapy, clinical evaluation and repeat biopsies are scheduled at defined intervals to detect progression to clinically significant disease at a stage at which it can still be effectively treated with surgery or radiotherapy. While not right for all patients with low risk prostate cancer, active surveillance should be considered a viable management strategy that is endorsed by the American Urological Association and has been incorporated into existing national best practice guidelines.
There is also growing interest in modifiable factors that may influence the behavior of disease in patients who choose to defer initial treatment. The Men’s Eating and Living (MEAL) Study, a clinical trial designed to evaluate how diet and nutrition impacts prostate cancer outcomes in patients managed with active surveillance, is currently open and enrolling patients at Fox Chase Cancer Center.
Unfortunately, the perils of over diagnosis will not be solved with re-classification. Rather than assuming all Gleason 6 tumors are created equal and should be dismissed as IDLE, improved patient-provider risk communication may prove to be a more effective means of reducing the harms of over treatment.
